Essay by Ron Merkin. All names, except the author’s, have been changed.
Part One: Drugs
“How do you feel about the use of psychotropic medication in the treatment of psychiatric patients?” she asked.
Her question caught me completely unprepared.
It was my first day on the job as a psychiatric social worker. No interview had been required before I began work because I’d switched from a pediatric to a psychiatric hospital setting, and both were under the umbrella of the New York City civil service system. So, having met my supervisor-to-be a minute or two before this question and having no idea about her feelings on the issue, I found myself facing her across her desk while staring clueless at the air in front of me.
“Don’t worry about saying what you think I want to hear,” Beatrice encouraged me. “I sincerely want to know your feelings about drugs.”
“Well…” I stopped. Psychotropic drugs were so heavily relied on…
“I value your opinion,” she insisted.
“Well… frankly…”
“Oh, come on. You’re entitled to an opinion! It helps us get an idea about your leanings as part of our staff. I need to know how you feel about…”
“OK,” I surrendered. Then, fast, as if something in me wanted to get this over with: “I don’t agree with drugs.”
Without a pause – not even for a second – she erupted, “How dare you say that?”
It only occurred to me later that she might have guessed what I’d say in advance.
“Who do you think you are? Your first day at work on a psychiatric ward and you think you know better than our psychiatrists?” (I did, but thought maybe I’d better not mention that.) “Why, drugs are a miracle!” she ranted.”We wouldn’t be able to function without them!” (Without saying anything, I mentally substituted the word control for function.)
It was the late 1970s. Because all this happened so long ago I don’t remember how long our “conversation” lasted. But when Beatrice seemed satisfied that she’d finally set me straight, she gave me a key to the locked ward a short walk down the hall from our office. With this I’d be able to let myself in and out.
Accompanying me there that first time, she said she’d introduce me to the staff. It was also an opportunity for me to get an impression of the patients in the large community room where most congregated during the day.
Once in the ward, we passed a young man who was shaking uncontrollably while trying to stand up straight. Before I could ask what was wrong, Beatrice explained, “That’s nothing to worry about. Especially when patients first begin drug therapy, the doses prescribed may be too potent. It can take a while before our psychiatrists’ experiments arrive at the right balance.”
She introduced me to four nurses who sat next to one another behind an elongated barrier station that separated the community room from the off-limits staff-only area. Then we proceeded to the psychiatrists’ offices. The two psychiatrists – a woman and a man, both young – happened to be discussing something in the man’s office when Beatrice knocked on his door.
“It’s convenient that you’re both in the same place,” she said.
Inviting us in, the psychiatrists shook my hand and welcomed me aboard. Then the man asked Beatrice if she’d already decided which patients to assign to me.
“Not yet,” she answered.
“Then I suggest Robert Smith and Julia Nordic.”
No background histories or diagnoses were proffered. When I asked about that, Beatrice mentioned that the psychiatrists were busy but that she’d fill me in on that sort of thing later.
She never did, but I found the information easily enough by reading a written log that all therapists had access to. When I arrived the next morning, I let myself into the ward and asked one of the nurses to point these patients out.
“They’re not here yet. Both usually come to the community room late,” she told me. Then, looking puzzled, she suggested I talk with the head of the social work department first. “He’s waiting for you.”
Noticing my puzzlement, she continued, “Didn’t Beatrice tell you? He wants to talk with you. I thought you knew. His name is Herb Riley. Third floor, room 12.”
Sitting behind his desk, the head of the social work department didn’t ask me to have a seat. With a chair unoccupied to his left, he instead dove right in while I stood the entire time: “Beatrice told me you don’t approve of drug medication.”
Oh, God, another lecture? I thought. A replay – emotional harassment, another admonishment?
“Is that correct?” Herb was asking me.
“I think you know that yesterday was my first day on the job,” I responded. Then, telling him exactly what had transpired between me and Beatrice, I noticed a knowing expression come over his face.
“Oh now I understand. Don’t worry about it. I’ll talk to her. I’ll take care of it.”
If he did, he wasn’t successful. My fourth day on the job, Beatrice informed me we’d be meeting with the two psychiatrists the next afternoon.
She hadn’t mentioned a word about drugs since I’d been called to the chief social worker’s office two days before. So imagining that Herb’s talk with her had indeed worked and an orientation lasting longer than my brief introduction to the psychiatrists three days ago was routine for new employees, I was dumbfounded when, as I sat in Dr. Welbroth’s office that Friday, no one said anything to begin the meeting.
It seemed to me that at least a minute passed. Finally, one of the psychiatrists said, “Beatrice, why did you want to have this meeting?”
A nightmare that fades but always recurs: “I want you to tell him how indispensable drugs are in the treatment of mental patients,” she said. “He thinks they’re unnecessary and should not be used.”
Silence. An awkward atmosphere. Then slowly – like a cautionary, very bit-by-bit “testing the waters”-type process – the psychiatrists and I launched one of the most fascinating, fun and enjoyable conversations about mental health that I can remember to this day. Freud, R. D. Laing, Thomas Szasz, our own hypotheses, even drugs: eventually, any topic we came up with was evaluated, discussed, even laughed about to the fullest.
This lasted about an hour. With a mixed expression of double-crossed-plus-totally-uninterested, Beatrice hadn’t said a word.
I can’t say I got along with Beatrice the rest of my time at this hospital. But especially because it must have been hard for her, I appreciated the occasional compliments she eventually gave me about the strange, risky, alternative experiments I attempted in an effort to help patients assigned to me and sometimes to someone else.
Part Two: “Psychotherapy”
The two-year curriculum required to get a master of social work degree included a “field placement” assignment in a different clinical setting each year. Working in the psychiatric ward of a VA hospital during my second year, I learned that almost all the patients there were young men who had served in Vietnam. Every one of them hallucinated. In spite of that, talk therapy worked.
To my surprise, it didn’t with patients I had a few years later at the hospital described above. For some reason I’ve never understood, patients in this second facility seemed so deeply entrenched in their hallucinations that they couldn’t communicate in what seemed to me standard everyday conversation. One example was Julia, the young woman Dr. Welbroth suggested I be assigned to in Part One.
Because patients were not allowed out of the locked ward, all therapy sessions had to be done in the patients’ community room. My daily “How are you today?” greetings while attempting to launch sessions with Julia were always answered the same: “I’m not Julia. Julia’s dead. Can’t you see her? She’s lying on the floor right in front of you!”
That, plus similarly unproductive interactions with other patients, made me realize that verbal psychotherapy was a waste of time. So I started wondering how else I could reach these people.
Walking to the subway after work one day, I noticed a sign in the window of a bank inviting passers-by to come in and enjoy a free live classical music concert in the lobby. Having entered and found a comfortable seat, I wondered if the music might somehow help me connect with some intuitive insight about how to help Julia.
I can’t remember exactly how the following occurred, but thinking I “heard” an instruction, I tried to picture my entire being descending to my stomach. Once there, I felt coaxed to “give Julia a task, something concrete. It can be simple, like telling her she’s required to find you and say ‘Hello, Mr Merkin’ wherever you are at at several exact times during the day. Be sure at those times that you’re far enough away to make this seem like a challenge but close enough so she can find you.”
Julia smiled – broadly, the first time I’d noticed that – as I explained the rules of this game the next morning. Still smiling, she was always exactly on time to deliver her greeting every hour (the time span I decided on). Not only that, she stopped hallucinating and didn’t begin again for the next three days. Noticing that, the psychiatrists decided to discharge her.
I was aware of space shortages, but her and others’ discharges without any resolution to family problems and other external issues in their lives virtually guaranteed returns to hospitalization. Agreeing with me, the psychiatrists I spoke with about this discharged her anyway.
An even more outlandish effort that worked (at least until he, too, was discharged) concerned Edward. He spent almost every day reciting the Catholic “Hail Mary” prayer while pacing back and forth for hours (and I mean hours) in the hallway outside the rooms where patients slept. So, “descending to my stomach” again, I heard that, to reach this guy, I should imitate him by walking to his side while reciting over and over the same prayer he was repeating.
But might this be dangerous? Might he get angry and pounce on me? For some reason I decided to take a chance.
I can’t remember how many “Hail Mary” walks back and forth I did before, finally looking at me, Edward erupted in laughter. It became so hysterical that he collapsed on the floor. A nurse came to see what was going on.
“He’s ventilating,” I told her. “There’s nothing wrong. He doesn’t need medical attention.”
Partly because Edward stopped his pacing after that, he too was discharged. Unfortunately, walking in Times Square a few weeks later, I saw him on his knees praying in front of a porn shop. He didn’t notice me, and I was late for an appointment, so I didn’t stop to talk with him.
I can’t remember how long after this I quit my job at this psychiatric hospital. Never understanding all my reasons, I suspect that one was feeling let down by cases like Edward’s. As I look back, I can’t help wondering anyway whether it was the outlandish techniques themselves or the patients’ perceptions that someone actually had gone to the trouble of devising individualized methods to get through to them that accounted for the temporary “cures.” My attempts weren’t the same as prescribing drugs, drugs, and more drugs to patient upon patient, after all.
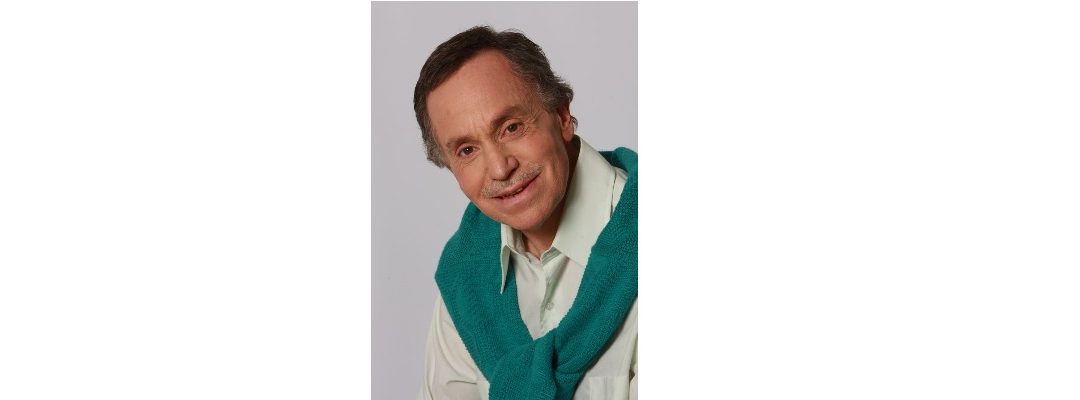
Ron Merkin is a retired psychiatric social worker, journalist, fiction writer and entertainer. He lives in Montpelier.